Diabetic Neuropathy – ಮಧುಮೇಹದ ನರಗಳ ನೋವಿಗೆ ಕಾರಣಗಳು
Diabetes and peripheral nervous system
Diabetes can affect the peripheral nervous system, leading to a condition called diabetic neuropathy. This occurs as a result of prolonged high blood sugar levels damaging the nerves, leading to symptoms such as numbness, tingling, and pain in the hands and feet. In severe cases, diabetic neuropathy can also cause muscle weakness and difficulties with coordination and balance. Effective management of blood sugar levels can help to prevent the development of diabetic neuropathy and its progression.
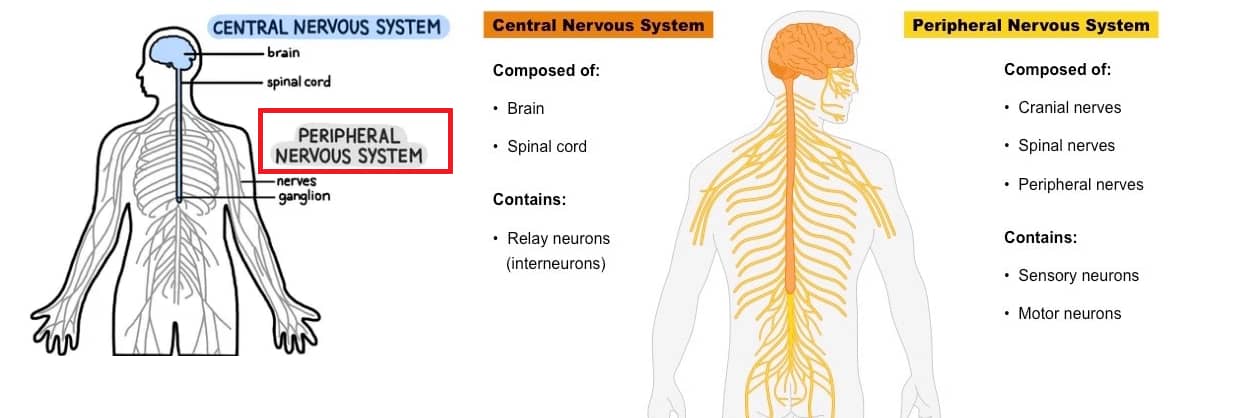
What is peripheral nervous system (PNS)?
The peripheral nervous system (PNS) is the part of the nervous system that is outside the brain and spinal cord. It is responsible for transmitting sensory information from the periphery of the body to the central nervous system (CNS), and for transmitting motor commands from the CNS to the muscles and glands. The PNS is divided into two branches: the somatic nervous system and the autonomic nervous system. The somatic nervous system controls voluntary movements, such as those involved in walking, and the autonomic nervous system controls unconscious functions, such as those involved in regulating heart rate and digestion.
Diabetic neuropathy is a type of nerve damage that can occur in people with diabetes. It is caused by high blood sugar levels damaging the nerves over time. There are several different types of diabetic neuropathy, each affecting a specific area of the body:
Peripheral neuropathy: affects the nerves in the extremities, causing numbness, tingling, and pain in the hands and feet.
Autonomic neuropathy: affects the nerves that control internal organs, such as the heart, bladder, and digestive system, causing a range of symptoms including digestive problems, incontinence, and impaired sweating.
Proximal neuropathy: affects the nerves in the legs and hips, causing weakness and pain in the thighs, hips, or buttocks.
Focal neuropathy: affects a single nerve or a group of nerves, causing sudden weakness or pain in specific areas, such as the face, torso, or leg.
How to treat?
Treatment for diabetic neuropathy typically involves a combination of measures to control blood sugar levels, manage symptoms, and prevent further nerve damage. Some common treatments for diabetic neuropathy include:
Blood sugar control: Effective management of blood sugar levels is crucial for preventing the progression of diabetic neuropathy. This can be achieved through a combination of diet, exercise, and medication.
Pain management: Over-the-counter pain medications, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), can help relieve symptoms of diabetic neuropathy. In more severe cases, prescription pain medications or nerve blocks may be necessary.
Vitamin and mineral supplements: Taking vitamin B1 (thiamine) supplements can help improve nerve function and reduce symptoms of neuropathy.
Physical therapy: Gentle exercise, such as walking or swimming, can help improve circulation and relieve symptoms of neuropathy. Physical therapy can also help maintain muscle strength and improve balance.
Topical treatments: Capsaicin cream, made from chili peppers, can be applied topically to relieve neuropathic pain.
Neurostimulation: Transcutaneous electrical nerve stimulation (TENS) and spinal cord stimulation are two neurostimulation techniques that can help relieve neuropathic pain.
Surgery: In severe cases, surgery may be necessary to relieve pressure on nerves or repair nerve damage.
It’s important to work with a healthcare provider to determine the best treatment plan for diabetic neuropathy. Regular monitoring and follow-up care is also crucial to ensure the best outcomes.

